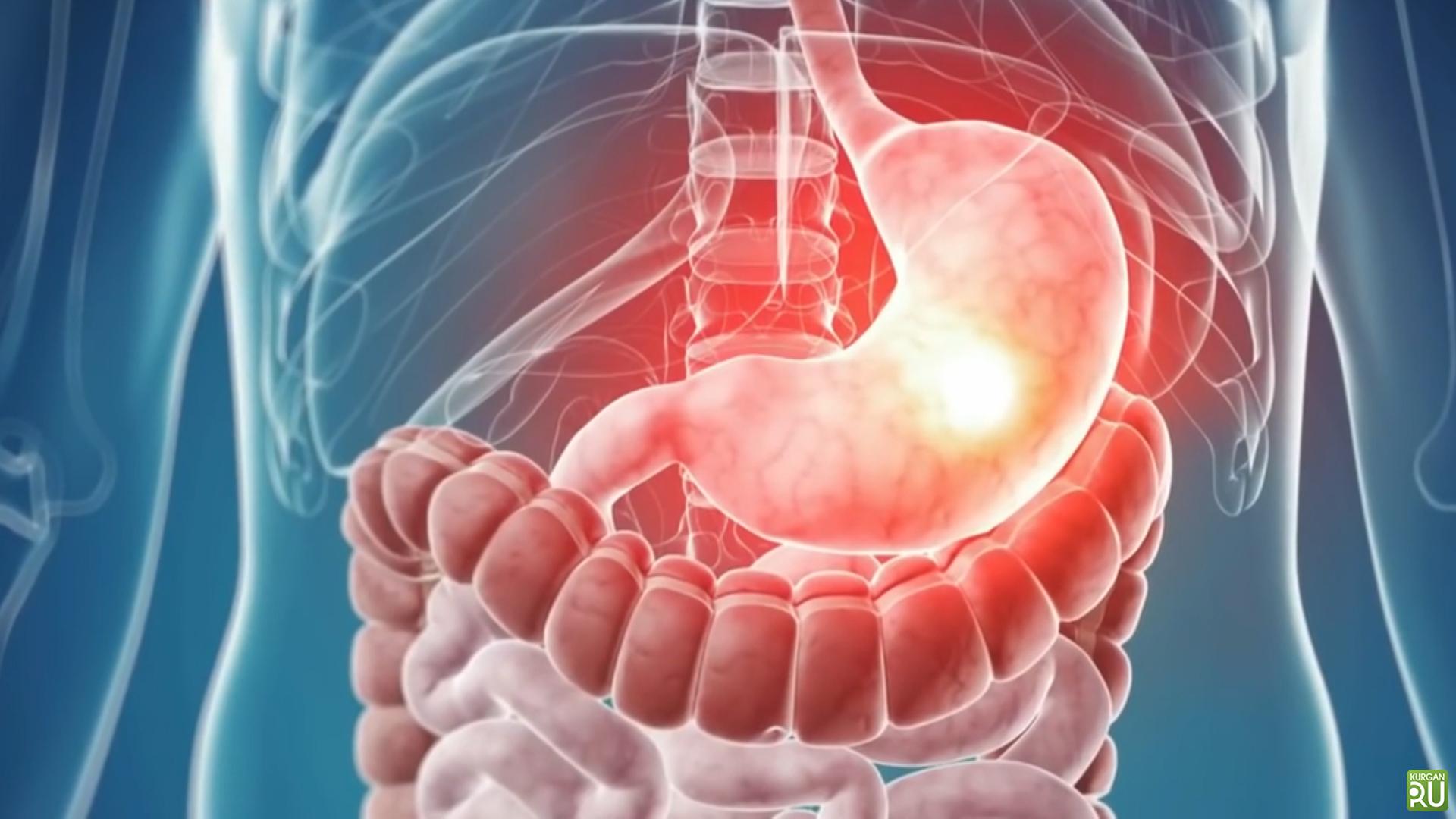
Stomach Diseases – Causes and Treatment
This results in gastritis. Gastritis often presents with symptoms such as abdominal pain, nausea, and heartburn. It is not a serious disease and can be easily treated with proper nutrition and medication.
What causes gastritis?
The most common cause of gastritis is infections caused by bacteria called Helicobacter pylori. Other causes of gastritis include:
- Smoking
- Excessive alcohol consumption
- Long-term use of drugs such as aspirin, ibuprofen, known as non-steroidal anti-inflammatory drugs
- Physical stress: a person has a serious illness, major operations, serious injuries and burns
- Mental stress
- Infections of various bacteria, viruses or fungi
- Food allergies
- Radiation therapy
- Advanced age
- Food poisoning
- The immune system attacks its body cells: In this case, the disease is called autoimmune or type-A gastritis.
What are the symptoms of gastritis?
Symptoms of gastritis may occur differently in each patient. Some patients may not have any symptoms. The symptoms of acute and chronic gastritis are different.
Symptoms of acute gastritis
Sudden abdominal pain is typical for acute gastritis. Pain is increased by hand pressure on the area. Other symptoms of acute gastritis include;
- Back pain
- Nausea, vomiting
- Loss of appetite
- Continuous belching
- Feeling fullness in the abdomen
- Bloating
- Bloody or coffee grounds vomiting
- Blood or black stool in stool
- Heartburn can be sorted as follows.
Symptoms of chronic gastritis
Most patients with chronic gastritis do not feel any symptoms for a long time. Some patients have mild symptoms such as bloating, fullness, and belching. But if left untreated; stomach ulcer, duodenal ulcer or stomach cancer.
What is antral gastritis?
Gastritis, according to localization in the stomach;
- pangastritis
- Antral gastritis
- It is classified as corpus gastritis.
Gastritis, which is seen in the section just before the exit of the stomach called antrum, is called antral gastritis. Antral gastritis can occur in acute or chronic form and its symptoms are shaped accordingly. It is the most common form of gastritis and 80% of all gastritis occurs in this type. Antral gastritis is usually caused by Helicobacter pylori.
What is chronic gastritis?
The often recurrent or prolonged inflammatory state of the gastric membrane is called chronic gastritis. Chronic gastritis is usually asymptomatic or causes mild discomfort with symptoms such as belching or bloating after meals. Chronic gastritis occurs for different reasons and is classified as type A, B or C according to the causes:
1) Type gastritis (Autoimmune gastritis): It is a type of chronic gastritis that occurs as a result of the body’s immune system attacking the gastric mucosa cells.
2) B type gastritis (Bacterial gastritis): It is a type of chronic gastritis caused by bacterial infections. Helicobacter Pylori is responsible for most of this group of gastritis.
3) Type C Gastritis: Caused by chemical or toxic substance irritation. It usually develops due to long-term drug use. Other triggers for type C gastritis include excessive alcohol consumption or rarely biliary reflux. Biliary reflux is a condition in which bile fluid escapes from the duodenum to the stomach.
How is gastritis diagnosed?
Firstly, a detailed history is taken from the patient for diagnosis. The patient’s complaints, medical history, medication, eating habits, alcohol, and smoking are questioned in detail.
Then physical examination is performed. Physical examination examines the abdominal pain for signs of increased pain. The upper abdomen is then examined by ultrasonography.
X-rays are only taken if there is suspicion of perforation in the stomach. Endoscopy should be performed for a definitive diagnosis. Endoscopy is performed by examining the stomach by entering the mouth with a tubular device with a lighted camera at the end. If necessary during the endoscopy, tissue samples are taken from the stomach.
Blood tests can be performed to detect inflammation and pathogens in the body. For example, if autoimmune gastritis is present, antibodies to components of the stomach cells can be detected in the blood. A stool examination can also be performed. In gastritis-related bleeding, blood is detected in the stool.
How to treat gastritis?
Gastritis can usually be treated with changes in habits and nutritional measures without the need for any medication. When these changes are not sufficient, various medications are used in the treatment.
- The first step in the treatment of gastritis is to stay away from everything that irritates the lining of the stomach. Therefore, coffee, alcohol, and cigarettes should be left.
- If the symptoms are severe, it may be beneficial not to eat for a day or two. As a rule, loss of appetite occurs during periods of exacerbation of gastritis.
- If the symptoms are slightly milder, lightly digestible light foods should be consumed as small meals.
- Relaxation methods such as meditation or progressive muscle relaxation techniques may help in cases of gastritis triggered by stress.
Gastric acid-suppressing antacids, proton pump inhibitors, H2 receptor blockers are used in the treatment of gastritis. In cases of Helicobacter pylori and other bacteria, antibiotic treatment is initiated. Chronic autoimmune gastritis is often associated with vitamin B12 deficiency. Therefore, vitamin B12 injections are also used in the treatment of autoimmune gastritis.
Gastritis diet
Diet is an important part of gastritis treatment. It is recommended that foods consuming Helicobacter pylori bacteria be consumed regularly in the gastritis diet. For this purpose, homemade yogurt, sauerkraut, tarhana probiotics such as can be consumed. With the ingredients in broccoli content, garlic has broad-spectrum antibacterial properties and has a lethal effect on Helicobacter pylori.
Also, research has found that ginger, apple cider vinegar, turmeric, oregano cranberry juice, pineapple, green tea, carrot, and beet juice both improve gastritis and alleviate symptoms such as nausea, stomach pain, burning, bloating and heartburn.
What foods are good and not good for gastritis?
Gastritis was good from food and drinks;
- Fresh fruits and vegetables
- High fiber foods such as apples, oatmeal, broccoli, carrots, and beans
- Whole grains
- Coconut oil
- Low-fat foods such as fish, chicken and turkey breasts
- Probiotics such as tarhana, homemade yogurt, and sauerkraut are available.
Some of the foods and drinks that trigger gastritis are;
- Chocolate
- Coffee
- Alcohol
- Acidic foods such as tomatoes
- All kinds of processed food
- Food and beverages containing high fat and sugar
- Fried foods
- Food and beverages containing artificial sweeteners
- Extremely spicy foods
- Frozen foods.
What is Duodenitis? Causes, symptoms, and treatment of duodenitis
WHAT IS DUODENITIS?
Duodenitis or inflammation of the duodenum, also known as the duodenum, is the beginning of the small intestine inflammation. Inflammation of the duodenum can cause abdominal pain, bleeding and other gastrointestinal symptoms.
The most common cause of duodenitis is gastric infection associated with a bacterial species called Helicobacter pylori (H pylori). This organism normally disrupts the mucus barrier that protects the delicate duodenal lining from acidic stomach contents. Loss of this barrier causes chronic inflammation and duodenal ulcer.
Many people are infected with H pylori at a young age, but the symptoms do not occur until adult age. In some people, H pylori infection causes duodenitis; if not treated, it may lead to ulceration of the duodenum. Serious and prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as alcohol or tobacco, may also lead to duodenitis. Less commonly, Crohn’s disease can cause duodenitis.
Acute duodenitis is called chronic duodenitis if symptoms occur suddenly and become uncomfortable for a short period if they occur for long periods of months or even years.
SYMPTOMS OF DUODENITIS
The signs and symptoms of duodenitis may be fixed or sporadic and the course of the disease varies between individuals. If the cause is H pylori, your symptoms will remain until the infection is treated. Some people with duodenitis have no symptoms, others may have burning pain or nausea with or without vomiting.
CAUSES OF DUODENITIS
Duodenitis is often caused by bacteria called Helicobacter pylori (H pylori). The following may also cause duodenitis:
- A bacterial, fungal or viral infection
- Severe illness or stress
- NSAIDs, aspirin or steroid medication
- Use of tobacco products or alcohol
- Crohn’s disease
- Radiation for cancer treatment
- Injury to the stomach or small intestine
- A toxic object that you swallow like a button cell
DUODENITIS TREATMENT
In the case of H pylori-associated duodenitis, the infection can be successfully treated with antibiotics. In duodenitis not associated with H pylori, drugs that reduce stomach acidity can be an effective treatment. You can reduce your risk of H pylori infection by following common hygiene practices, such as washing your hands with soap and water.
Lifestyle changes, such as limiting alcohol consumption and limiting your use of nonsteroidal anti-inflammatory drugs (NSAIDs), can reduce your risk of non-H pylori-related duodenitis.
Seek immediate medical attention for severe symptoms such as severe abdominal pain, bloody or black tar stools, or bloody or black vomiting.
What is reflux? What are the symptoms and treatment?
Many people have symptoms of indigestion, souring and burning of the esophagus after eating. This disturbing condition is evident with food and gastric acid from the esophagus and even the mouth. This situation is temporary in some people and disappears at a certain time.
However, in some people, it becomes quite uncomfortable, often occurring and quite painful. This disease was called “gastroesophageal reflux”. It is a very common disease (15-20%). Although it is more common in women, severe esophageal damage is more common in men. It can cause serious conditions in the elderly and children.
Symptoms of reflux
The most common symptom is heartburn. Some people may feel this burning in their stomachs, neck, shoulders or even on their back and arms. It is sometimes indistinguishable from heart pain. They usually consult a doctor for this reason.
Reflux esophagitis was found in 50% of the patients who had negative coronary angiography for chest pain. In esophagitis, pain is often acute onset and lasts for hours, awakens from sleep, is associated with antacids and food, is associated with food and meals, is felt in lying on your back and bending forward, in 50% of cases it is accompanied by symptoms such as pyrosis, regurgitation, and dysphagia, often unrelated to exertion or sternum. felt in the back region, does not spread.
In addition to pain, sour water is another common symptom of “regurgitation”. Leaves a bad taste in the throat and mouth, usually occurs after meals rarely during meals. Symptoms often occur while lying and sleeping. Other symptoms include abdominal distension, burping, hiccups, tickling, chronic cough, halitosis, hoarseness, nodules in the vocal cords, and asthma attacks.
Treatment of reflux
Reflux disease is a disease that can be prevented and treated after being diagnosed. With the meal, the secretion of acid begins in the stomach for the grinder process. At the end of the meal, some of this secreted acid overflows from the stomach and irritates the esophagus. We call this backflow overflow. Reflux acid can cause temporary and permanent damage to the esophagus. We use the definitions of burn heartburn ağrı as a result of this irritation and Öz esophagitis ada for damage to the esophagus.
The stomach surface is accustomed to acid and has mechanisms to eliminate the destructive effect of acid. However, there are no such protective mechanisms against acid in the esophagus. Normally, there is a mechanism between the stomach and esophagus that acts as a gate that we call the “lower esophageal sphincter”.
This door allows the ingested bites to pass through the esophagus into the stomach but operates with a mechanism to prevent the stomach contents from escaping back. Relaxations or disturbances in this gate (gastric hernia-hiatal hernia) are the causes of reflux disease.
In cases where the pressure in the stomach is increased (eating too much, after meals, etc.), the frequency of reflux is higher.
Which patients require reflux surgery?
- Age (the younger the patient, the more priority is surgery).
- Severity, frequency, type of complaints
- The severity of damage to the esophagus
- Rate of disease recurrence despite drug treatment
- In the case of gastric hernia (Hiatal Hernia) with reflux, the patient is treated with surgery.
What is corrected with reflux surgery?
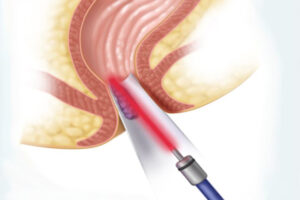
Nowadays, we benefit from the advantages of laparoscopic surgery in the treatment of reflux disease.
Laparoscopic fundoplication operations, which aim to reconstruct the gate between the esophagus and the esophagus of the impaired lower esophageal sphincter, are widely used all over the world. Surgery is a laparoscopic procedure performed by using the latest technical developments.
It is a procedure in which the patient can take oral feeding the next day and can be sent home on the same day or the next day and can work within 7 days. All the advantages of laparoscopic surgery (such as less pain, shorter hospital stay, and no postoperative risk) are utilized.
Thus, for years and every day, the elimination of drug intake, the regression of inflammatory events in the esophagus and the removal of the cancer risks associated with them, provide a better quality of life for the patient. The side effects of these laparoscopic fundoplication procedures performed by experienced surgeons are minimal and the success rate is between 95-100%.
It is a recommended operation with appropriate patient selection as a result of the joint evaluation of gastroenterology and surgeons.
What are the symptoms of reflux (GER)?
The most important symptom of GER is burning upward in the chest. Burning can be felt in the stomach, throat or neck. Especially alcohol, pickles, chocolate, sour, bitter and spicy foods are among the foods that intensify the burning. Another important symptom is the involuntary ingestion of gastric fluid without nausea. This feature is distinguished from vomiting.
Once or more times a week, a burning throat in the chest and bitter-sour water into the mouth is sufficient for the diagnosis of the disease. Apart from these two important symptoms.
Symptoms of reflux due to the irritation of other organs are also important in the diagnosis of GER.
- Persistent coughing
- Hoarseness
- Polyp or nodule in vocal cords
- Throat infections such as untreated laryngitis and pharyngitis
- Feeling fullness in the throat
- Frequent need for throat clearing
- Asthma not responding well to treatment
- Recurrent pneumonia
- Reflux should be suspected as the underlying disease in short-term breathing stops during sleep.
The need for continuous throat cleaning, muting, reflux is the main cause in most people with frequent pharyngitis or laryngitis. Again, half of those with chronic cough have been found to have reflux disease. There are even patients who cough for years and go the doctor to doctor without a diagnosis. Asthma and reflux together make one worse. Some patients with suspected reflux have chest pain that is impossible to separate from heart pain. In such cases, it is best to suspect reflux after the first cardiac examination.
Difficulty in swallowing, painful swallowing, bleeding in the stomach or weight loss may be signs of reflux or may indicate a completely different disease. Reflux disease in children is in the form of simple vomiting but may be responsible for “sudden child death” syndrome, especially in infants. Posture disorder in childhood, growth and developmental retardation, anemia, pneumonia attacks, respiratory diseases, strangulation attacks in newborns are among the reasons for the presentation of GER. Reflux underlies one-third of childhood asthma.
What are the diseases caused by reflux?
- Growth and developmental delay in children
- Pneumonia due to gastric fluid leakage to the lung,
- Respiratory diseases such as laryngitis, pharyngitis, bronchitis, asthma,
- Esophageal inflammation,
- Peptic stenosis (narrowing of a part of the stomach),
- Digestive tract bleeding,
- Anemia,
- Barrett’s disease that causes esophageal cancer
- May cause cancer.
Treatment of reflux
There are two methods: drug treatment and surgical treatment. In the treatment of reflux, if there is no underlying organic cause, the patient is given anti-acidic drugs and acid-neutralizing drugs.
Surgical treatment of surgery between the stomach and the esophagus muscle is strengthened Generally if there is a gastric hernia is sometimes applied when the drug treatment can not be obtained. In patients who do not want to use the drug for a long time, if surgical treatment is appropriate and the patient can be applied. The patient should be informed about the side effects and complications of surgical treatment.
Reflux disease is a chronic disease, from time to time complaints may increase, decrease, disappear and recur. Therefore, there are rules that the patient must follow to prevent reflux.
Ways to prevent reflux
- Lie on a high pillow (the upper body and head should be high when lying down).
- Avoid eating too much (Excessive food increases stomach pressure and increases the likelihood of reflux).
- Eat a small amount of frequent and regular meals.
- Eat food slowly and chew well.
- Reduce fat (avoid fries, fast food foods and margarine. Over-fat foods also have a high gastric residence time and more gastric acid is released).
- Avoid chocolate (Methylxanthine in chocolate loosens the muscles in the esophagus, causing relaxation in the sinker).
Continue
- Avoid coffee and drink less tea (caffeinated or careless coffee increases the likelihood of reflux).
- Avoid substances that irritate the esophagus.
- Do not drink acidic beverages, canned fruit juices, such as alcohol, cola, soda pop.
- Avoid very spicy foods, pickles and vinegar (Spices can increase the severity of reflux and increase stomach burnings. Therefore, limit the spicy prepared foods and use fewer spices in your meals.
- Do not lie down immediately after a meal, sit for at least 1 hour.
- Avoid drinking (Alcohol increases stomach acid).
- Avoid cigarettes and other tobacco products (Nicotine loosens the astringent at the bottom of the esophagus).
- Do not gain weight (obesity increases reflux complaints).
- Try to avoid stress as much as possible.
- Since fluid consumption increases stomach pressure, take it between meals, not during meals.
- Try not to wear tight clothes, especially after a meal.
What is an ulcer? What are the symptoms and treatments?
The ulcer is the loss of tissue caused by the destruction of the stomach or duodenum (duodenum) by gastric acid and digestive fluids (eg, pepsin). Tissue loss can go deeper with the effect of acid pepsin. Inflammation creates a wound.
What causes the ulcer?
The biggest cause is a micro pot called “Helicobacter pylori” and the regular intake of NSAIDs (aspirin, antirheumatic drugs). Other possible causes include genetic predisposition, all kinds of stress, cortisone drugs, alcohol, smoking, coffee habit, environmental pollution.
In which age range is the ulcer frequently seen?
The percentage of current ulcer patients (new or undergone) at any given time in our society is 2-6%. Duodenal ulcers are more common than gastric ulcers. Duodenal ulcer is more common between the ages of 30-50 and is 2-4 times higher in men than in women. Gastric ulcer is more common after 60 years of age and is more common in women.
What are the symptoms of an ulcer?
The most common symptom is a pain in the upper abdomen in the form of gnawing and burning. Usually occurs between meals. It can wake the patient from sleep at night (mostly in duodenal ulcer). With food and antacid, a chewable tablet that neutralizes stomach acid and lozenges, the pain is relieved from a few minutes to a few hours. The frequency of pains increases in autumn and spring. Less common symptoms in ulcer patients include nausea, vomiting (especially when pain is present, pain reduction or cessation of vomiting is very typical), loss of appetite and weight loss.
What are the dangerous consequences of ulcers?
BLEEDING
Ulcers are the major cause of upper digestive system bleeding. Sometimes it can be seen even in people who have never had stomach pain before. They vomit “coffee grounds” colored material or “tar colored” black stool stools. Persons who notice that their stool is black without further symptoms must contact an emergency health center immediately. Sudden malaise before vomiting and black feces should be suspected of upper gastrointestinal bleeding in cold cold sweating.
PERFORATION (Stomach perforation)
It is the increase of the depth of the existing ulcer and the penetration of all the stomach-duodenum layers. Sudden and severe pain occurs when the stomach acid-pepsin content passes through the abdominal cavity. The abdomen hardens like wood, it becomes difficult to move and walk because of pain. Treatment is usually surgery.
Occlusion
Acute ulcers in the duodenum and pylori can cause tissue edema (swelling), resulting in the formation of scar tissue as a result of deep ulcers for a long time.
The patient vomits the material that he eats and accumulates in the stomach as a result of the continuous secretion of gastric juice. Vomiting is abundant and continuous.
Even if the patient eats, the food cannot pass to the organs without digestion (digestion – absorption – not in the stomach, but the duodenum and small intestine), there is constant weight loss. Diagnosis should be made as soon as possible and operated.
How is the diagnosis of ulcer done?
With physical examination and ultrasound, the ulcer does not show any signs. But it gives us a chance to rule out other diseases. Many doctors prescribe an acid-blocking medication, suggesting that after 2 weeks of medication, the symptoms do not improve, with no ulcers (from treatment to diagnosis).
There is practically no other diagnosis. For the diagnosis of ulcers, radiological examination of the upper digestive system or endoscopy of the upper digestive system (esophagogastroduodenoscopy) is required.
Ulcer treatment
STOMACH – DUODENUM GRAPH
During the passage of barium through the stomach, anatomic structure of the stomach and duodenum line is observed.
ENDOSCOPY (GASTROSCOPY)
It is the direct observation of the esophagus, stomach, and duodenum with a small, light, durable tube. Approximately anywhere in the organs to be seen can be observed clearly. The procedure is usually performed by administering medication to calm the patient. During the procedure, a biopsy can be taken for pathological examination and urease test. Biopsy does not cause any discomfort or pain.
DIET
In the past, spicy, bitter, sour, pickles, fatty and acidic foods should be avoided, milk treatment was said. Today, there is no special diet for ulcers or even the damage of milk before bedtime. Experiments have shown that a special diet does not contribute to ulcer healing.
It is said that the food that is currently thought to cause a personal complaint should be restricted. (For example, if a person with an ulcer does not touch an onion, it is OK to eat it). However, patients with ulcers should stop smoking (if they smoke too much).
Smoking has been shown to delay ulcer healing and cause frequent ulcer mixes. Usually, patients with ulcers should not take aspirin or similar rheumatism medication. Alcohol intake may impair superficial mucosal resistance, resulting in delayed gastritis and ulcer healing. In acute ulcers, it is beneficial not to take them.
MEDICINES
Drugs used in the treatment of gastroesophageal reflux and ulcers are H2 receptor blockers (Ranitidine, Famotidine, Nizatidine) and proton pump inhibitors (omeprazole, lansoprazole). They relieve symptoms by reducing stomach acids. Also, stomach ulcers by eliminating the effect of ulcers, provide healing. Protein pump inhibitors are more potent in reducing acidity than H2 receptor blockers. But they are more expensive. In patients with helicobacter pylori, protein pump inhibitors are effective in eradicating Helicobacter pylori in combination with antibiotics used.
OPERATION
Many ulcers heal with medication. If bleeding, stenosis (puncture), puncture occurs and does not respond to medical treatment, urgent surgery is necessary.
What are Helicobacter pylori?
Many ulcers occur with the presence of helicobacter pylori. The presence of Helicobacter pylori in duodenal ulcers was found to be nearly 100% higher. Because of the presence of people with Helicobacter pylori but no ulcer, other factors (eg heredity) should be considered in addition to the presence of helicobacter pylori. The presence of Helicobacter pylori is certain to cause involuntary gastritis except that it does ulcers. It is also claimed to cause stomach cancers.